HomeDivisionsLung DiseaseThymic cancer
There are two types of cancer of the thymus, thymomas and thymic carcinomas. Both types of thymus cancer involve epithelial tumors, which means they are located on the outside surface of the thymus gland.
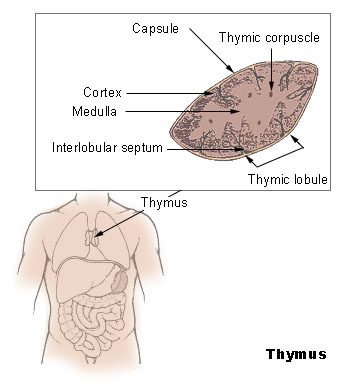
Anatomy of the Thymus
Image courtesy of National Institutes of Health
The thymus is not to be confused with the thyroid gland. The thymus gland is a small organ that lies under the breastbone in the upper chest area. It is part of the body’s lymph, or immune, system, which produces T-lymphocytes, or white blood cells. Their job is fighting infection. The thyroid gland is located in the neck near the Adam’s apple. It produces hormones that regulate bodily functions, including metabolism, breathing, heart and nervous system functions, body temperature, muscle strength, and more.
Both types of thymus cancer are rare. Based on data from the National Cancer Institute (NCI) Surveillance, Epidemiology and End Results (SEER) Program, the incidence is only 0.15 cases per 100,000 people for thymoma and 0.06% for thymic carcinomas.
Causes and Indications of Thymus Cancer
The etiology of thymus cancer is not fully known, but people with autoimmune diseases, such as myasthenia gravis, lupus, red cell aplasia, Good’s syndrome [hypogammaglobulinemia], rheumatoid arthritis, Addison disease, and others [see full NCI list of autoimmune disorders at: https://www.aarda.org/research_display.php?ID=47] are more likely to develop thymus cancer than other people.
Therefore, patients with autoimmune diseases may be routinely tested for thymus carcinomas, as many patients who do not experience symptoms, which include persistence cough, trouble breathing due to congestion or chest pain, may be ignored because they are associated with common illnesses.
Thymoma associated with autoimmune disease involves primary T-cell abnormality. Additionally, B-cell lymphonpenia, or low white blood cell count, has been observed in Good’s syndrome patients with thymoma-related immunodeficiency. Patients with thymoma-associated myasthenia gravis can produce autoantibodies to a variety of neuromuscular antigens. Some research indicates that oncologic outcomes are more favorable for patients with Myasthenia gravis than for other thymoma patients. The NCI, however, notes that there is conflicting data and suggests that the better outcomes may be due to early diagnosis in these patients, which allows for surgical removal while the tumor is still encapsulated. Additionally, Thymoma has been associated with an increased risk for second malignancies.
Common precursors to thymic lymphomas are T-lymphoblastic lymphoma, Hodgkin lymphoma, and primary mediastinal large B-cell lymphoma. . The majority of patients diagnosed with thymus cancer are between the ages of 40 and 60, however, thymic cancer typically occurs in younger patients. This form of thymus cancer is more aggressive than thymoma carcinoma and often has metastasized prior to diagnosis. Because thymic carcinoma patients often present with advanced disease, their five-year survival rate is 30% to 50%, according to SEER.
Pathology of the Disease
Thymoma carcinoma cells look like normal thymus cells, grow slowly and rarely spread to other organs. In fact, about 50% of patients with this form of thymus cancer are diagnosed while the cancer is localized inside the thymus capsule and can be surgically removed before it spreads to other areas of the body.
Thymic carcinoma, on the other hand, looks very different from normal cells, grows more quickly than thymic carcinoma, and usually has spread to other parts of the body before it is diagnosed. Therefore, this is the most dangerous and difficult-to-treat form of thymus cancer and has a higher risk of recurrence and death than thymoma cancer.
Diagnosis, Staging and Treatment
Initially, diagnosis involves physical examination to detect signs of disease, such as lumps or anything unusual. The attending physician will also review a patient history that includes lifestyle, past illnesses and treatments. The physician may order:
- A chest x-ray
- CT-scan (computed tomography) with contrast, which involves injection of dye to more clearly image organs and tissue;
- MRI (magnetic resonance imaging), which uses a magnet, radio waves and a computer to take detailed pictures inside the body; or
- PET scan (positron emission tomography scan), which uses radioactive glucose (sugar) to detect and image malignant tumor cells. Malignant show up brighter because they are more active and take up more glucose than normal cells.
- A biopsy of the tumor, however, is the only sure way to diagnose the disease. Therefore, thymus cancer may be diagnosed, staged and treated at the same time during surgery.
With biopsy, a fine needle is inserted into the tumor to remove a sample of cells. This core biopsy is microscopically viewed by a pathologist to determine if the tumor is malignant, and if so, which type of cancer is present and the stage of the disease.
Staging is the process used to determine if the cancer has spread, or metastasized, to other parts of the body. Cancer can spread to surrounding tissue or to other areas of the body through blood or the lymph system.
- Stage I – The cancer is encapsulated inside the thymus.
- Stage II – The cancer has spread into the fat around the thymus.
- Stage III – The cancer has spread to nearby organs in the chest, including the lung, sac around the heart or large blood vessels carrying blood to the heart.
- Stage IV – This stage is divided into two sub-stages IVA and IVB. With stage IVA, the cancer has spread widely around the lungs and heart, and with IVB, it has spread to the blood or lymph system.
Depending on the test results, the surgeon decides if all or part of the tumor can be surgically removed. If the cancer has spread, lymph nodes and tissues may be removed as well.
Standard Treatments for Thymus Cancer
The most common treatment for thymus cancer is surgery. But even if the surgeon removes all visible cancer cells, some patients may be given radiation therapy to kill any leftover cancer cells and lower the risk of the cancer returning. Chemotherapy may also be given prior to surgery to shrink the tumor. Drugs called corticosteroids may also be used, along with surgery, radiation or chemotherapy, to block hormones that feed growth and spread of cancer cells. Hormones are produced by glands and circulated in blood throughout the body.
New Treatments Under Investigation
Thymus cancer patients may also want to explore new treatment options under investigation and/or participate in clinical trials. Some clinical trials include only patients who have not yet started treatment, while others are for patients who have not responded well to treatment. Clinical trials may also test new ways to stop the cancer from recurring or reduce side effects of cancer treatments. Therefore, many patients can enter clinical trials before, during or after starting cancer treatment, depending on the goals of the clinical trial and patient status. The NCI provides a current, worldwide list of clinical trials for thymus cancer at: http://www.cancer.gov/cancertopics/types/thymoma.
Follow-up Care
Follow-up tests help the physician determine how well treatment is working, as well as to detect a recurrence of the cancer early. Some of the same tests performed to diagnose and stage the cancer may be repeated. Results of these tests help the physician decide whether to continue, change or stop treatment. After treatment ends, regular check-ups may involve follow-up tests to determine if the patient’s condition has changed or if the cancer has recurred.
Survival Rates
Physicians use thymus cancer survival rates to discuss a patient’s prognosis, or chance for recovery. Rates of survival are based on the five-year survival of patients from time of diagnosis and stage of the cancer. Because thymus cancer is so uncommon, accurate survival rates are not readily available, but the American Cancer Society offers these observed survival statistics from a large series of patients treated in Japan between 1990 and 1994.
Survival Rates for Thymus Cancer
| Thymoma | Five-year Survival Rate | Thymic | Five-year Survival Rate | |
| Stage I | 74% | Stage I | 74% | |
| Stage II | 73% | Stage II | 74% | |
| Stage III | 64% | Stage III | 33% | |
| Stage IV | 45% | Stage IV | 24% |
Courtesy of the American Cancer Society
Related Information:
Foundation for Thymic Cancer Research
What’s New in Thymus Research Topics?
International Thymic Malignancy Interest Group
PROFILE: Jennifer Marquez—Two-Time Cancer Survivor Beats Back Sarcoma
B-cell lymphopenia and hypogammaglobulinemia in thymoma patients
Neuromusclar disorder – myasthenia gravis
Surveillance, Epidemiology and End Results (SEER) Program
Technical Advances of Radiation Therapy for Thymic Malignancies
Learn About Clinical Studies
References:
National Cancer Institute
National Institutes of Health
American Cancer Society
Wikipedia.com
UCLA
University of Toronto
Medline.com
PubMed.com
Foundation for Thymic Cancer Research
American Autoimmune Related Diseases Association, Inc.