HomeDivisionsHeart DiseaseCoronary Heart Failure
ALL ABOUT CORONARY HEART FAILURE
Heart failure, also known as chronic or congestive heart failure (CHF), is the inability of the heart to efficiently pump enough oxygen-rich blood to meet the body’s needs. So, what is coronary heart failure? With CHF, blood moves through the heart and body at a slower rate than normal, starving the body of oxygen. This causes the heart chambers to stretch to hold more blood to pump, or become stiff and thickened. Heart failure occurs when the heart muscle eventually weakens and is unable to pump blood efficiently. The kidneys respond by retaining fluid, which backs up into the lungs and builds in feet, ankles and legs, causing swelling, or edema, of the extremities and other areas of the body. The body becomes congested, resulting in shortness of breath and fatigue.

The heart is located between the lungs in the middle of the chest and weighs between 7 and 15 ounces, or is just a little larger than the size of the person’s fist. Each day the heart beats on average 100,000 times and pumps about 2,000 gallons of blood By the end of a normal human lifespan, the has beat (expanded and contracted) more than 3.5 million times. Copyright healthinformation.com
Physiology of the Normal Heart
The heart has four chambers: the right and left atriums and right and left ventricles. When the heart functions properly [See Normal Heart Function], the body’s two largest veins, the superior and inferior vena cava, bring oxygen-poor blood to the heart’s right atrium, which passes through the tricuspid valve into the right ventricle. When the right ventricle is full, the valve closes and the right ventricle pumps blood into pulmonary artery, which has two branches to transport blood back to both lungs. Once in the lungs, the blood picks up oxygen, and carbon dioxide is expelled. The re-oxygenated blood is then transported through the pulmonary veins into the heart’s left atrium, and then passes into the left ventricle through the mitral valve. When the left ventricle is full, the valve closes and the left ventricle pumps the oxygen-rich blood throughout the body.
When the Heart Fails
There are two types of heart failure: systolic and diastolic dysfunction. Systolic heart failure is when the heart muscle becomes weak and does not contract with enough force to pump a sufficient supply of oxygen-rich blood to other parts of the body. With diastolic heart failure the heart contracts normally, but the ventricle–the heart’s pumping station–does not relax properly after the heart contracts, which reduces the supply of blood entering the heart and raises blood pressure in the lungs.
Type of heart failure is diagnosed with a test called ejection fraction, which measures the percentage of blood pumped with each beat, or contraction, of the heart. The ejection fraction is less than 40% in patients with systolic heart failure. With this type of heart failure, an echocardiogram (ECHO), or heart ultrasound, shows an enlarged heart.
With diastolic heart failure, the ejection fraction and the heart’s pumping capacity are usually normal, but the ECHO shows that the heart is not filling up with blood properly during the relaxation of the heart’s muscle between beats, or contractions.
Both types of heart failure starve the body of oxygen-rich blood and may involve the following symptoms:
- Shortness of breath
- Fatigue;
- Cough;
- Weakness or faintness;
- Loss of appetite;
- Frequent urination during the night;
- Waking at night due to shortness of breath;
- Tachycardia, a heartbeat faster than 100 beats per minute, irregular heartbeat or heart palpitations – the sensation the heart is pounding or racing; and
- Fluid retention, which causes weight gain, enlarged liver or abdomen, and swollen feet and ankles.
Causes of Heart Failure
Most people think of heart failure as a chronic disease that slowly evolves with aging, but heart failure can strike anyone at any age. It is true that heart failure is more prevalent in people over 65, as it is commonly caused by conditions that overwork the heart, including coronary artery disease (CAD), high blood pressure, heart valve disease, diabetes, thyroid disease, or a congenital heart defect.
But coronary heart failure may also result from:
- Heart attack, which results from a blood clot in the coronary artery that blocks supply of blood and oxygen to the heart and results in damage to heart tissue;
- Heart valve disease, which is caused by leaky or narrowed heart valves;
- Cardiomyopathy or weakening of the heart muscle as a result of an infection that involves the heart, drug or alcohol abuse, a genetic condition, or poisonous trace elements like lead and mercury.
- Some types of arrhythmias, or abnormal heart rhythms.
Other diseases that can cause or contribute to heart failure are:
- Amyloidosis, which is caused by abnormal proteins (amyloid) in the heart tissue that make it hard for the heart to work properly;
- Emphysema, or chronic obstructive pulmonary disease (COPD), which is caused by smoking or other environmental exposure that destroys the lung tissue overtime;
- Overactive thyroid, or hyperthyroidism, which is when the thyroid gland produces too much thyroid hormone
- Underactive thyroid, hypothyroidism, which is when the thyroid gland does not produce enough thyroid hormone,
- Sarcoidosis, which is caused by tiny clumps of abnormal tissue (granulomas) forming in certain organs causing inflammation in the lymph nodes, lungs, liver, eyes, skin, or other tissues; and
- Severe anemia, which is when the body fails to produce enough healthy red blood cells due to a deficiency of iron or certain vitamins [B12 and folate],
- Chronic infections, such as bacterial endocarditis, osteomyelitis, HIV/AIDS, hepatitis B or hepatitis C; inflammatory diseases of the heart or myocarditis, which involve infection induced by bacteria or a virus; certain cancers, including lymphoma and Hodgkin’s disease; chronic kidney disease; liver cirrhosis; and excess iron in blood.
Stages of Heart Failure
The American Heart Association and American College of Cardiology classify the stages of coronary heart failure according to a rating system that is based on the development and progression of the disease.
- Stages A and B – The person has not yet developed heart failure, but is at high risk due to the presence of coronary artery disease, high blood pressure, diabetes or other conditions that dispose them to developing this disease.
- Stage C – This includes people who have a condition called structural heart disease and have experienced or are currently experiencing symptoms of heart failure.
- Stage D – This includes patients who have advanced heart failure that is difficult to manage with standard treatments.
Treatments for Heart Failure
Treating heart failure involves medications and lifestyle changes. Severe heart failure may also require surgery or other procedures and medical devices that regulate heartbeat or give the heart a helping hand.
Medications
Medications prescribed depend on the type and severity of heart failure, as well as patient’s response to certain drugs.
- Diuretics, such as Lasix (furosemide), Microzide (hydrochlorothiazide), Thalitone (chlorthalidone), are prescribed to help reduce fluid buildup in lungs.
- ACE (angiotensin-converting-enzyme) inhibitors are given for high blood pressure and weak heart muscle. This group of drugs, which includes perindopril, captopril, enalapril, lisinopril and ramipril, lowers blood pressure by dilating blood vessels and decreases tension in blood vessels and blood volume to help the heart pump more blood. ACE inhibitors also reduce risk of heart attack.
- Aldosterone antagonists, like Inspra (eplerenone) and Aldactone (spironolactone), are diuretics given for heart failure. These drugs help the body get rid of salt and fluid through urine to lower the volume of blood the heart must pump.
- Angiotensin II receptor blockers (ARBs), such as Cozaar (osartan), Benicar (olmesartan), Micardis (telmisartan) and Diovan (valsartan), are used to treat CAD and may be used in place of ACE inhibitors to treat heart failure. Some ARBs, including Avalide (irbesartan and hydrochlorothiazide) and Hyzaar (losartan and hydrochlorothiazide), are combined with a diuretic. This group of drugs lowers blood pressure by inhibiting a substance that narrows blood vessels, which relaxes and dilates blood vessels so blood flows through vessels easily. They also activate certain hormones to release water and sodium through urine.
- Beta blockers, such as Lopressor or Toprol-XL (metoprolol), Inderal (propranolol) and Sectral (acebutolol), decrease the heart’s workload by slowing heart rate and lowering blood pressure.
- Vasodilators, including hydralazine and nitrates, work on different substances to dilate blood vessels and are often combined with other medicines to treat heart failure. Hydralazine is given along with a nitrate, such as Isordil (isosorbide dinitrate) or Imdur (isosorbide mononitrate), or BiDil, a combination of hydralazine with isosorbide dinitrate, may be given in place of an ACE inhibitor to treat heart failure, as well to relieve symptoms of angina, or chest pain.
- Digoxin helps a weak or injured heart pump blood more efficiently by strengthening heart contractions.
Lifestyle Changes
Lifestyle changes to improve heart failure include regular rest periods, exercise, a heart-healthy diet, weight loss if overweight and quitting smoking. A heart-healthy diet includes a variety of vegetables and fruits, whole grains, fat-free or low-fat dairy products, and foods high in protein (lean meats, egg whites, poultry and fish), nuts and seeds. Intake of sufficient dietary potassium, which is depleted by diuretics and other medications, and limiting intake of fluid and salt are essential for people with heart failure.
The heart needs potassium to conduct electrical impulses that cause it to contract. Low potassium, or hypokalemia, may cause heart palpitations or arrhythmia, which may result in sudden death. Potassium also helps to lower systolic [the top number] blood pressure by about eight points and may affect cholesterol level. Muscle cramps are symptomatic of low potassium, but people taking diuretics should have regular blood tests to check potassium level. A normal potassium level is 3.5 to 5 milliequivalents per liter of blood.
For a list of high-potassium foods visit the American Nutrition Association website. For more information on following a health-healthy diet, visit Your Guide to Lowering Your Blood Pressure With DASHby the National Heart Lung and Blood Institute and ChooseMyPlate.gov, on the U.S. Department of Agriculture website.
Surgery and Other Medical Procedures
As heart failure progresses and medications and lifestyle changes no longer control symptoms, surgery or other medical procedures may be recommended.
With severe heart failure, the right and left sides of the heart may no longer contract at the same time, disrupting the heart’s pumping action or heartbeat. An implantable cardiac resynchronization therapy (CRT) device, a type of pacemaker, or implantable cardioverter defibrillator (ICD) may be recommended to correct this problem. The CRT sends tiny electrical impulses to heart muscle to resynchronize contractions of the ventricles, which helps the heart pump blood more efficiently. An implantable cardioverter defibrillator (ICD) shocks the heart when an abnormally fast, life-threatening heart rhythm is detected to prevent sudden cardiac arrest, or death, to initiate normal heart rhythm. A CRT defibrillator (CRT-D), which combines defibrillator act with CRT function, may be recommended for some patients.
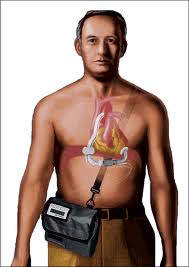
More radical procedures may be required for people who continue to experience severe heart failure symptoms at rest, despite other coronary heart failure treatments. These procedures may include a ventricular assist device (VAD) or heart transplant.
A VAD is a mechanical heart or circulatory device used to partially or completely replace heart function. VADs are designed to assist either the right ventricle (LVAD) or left ventricle (LVAD) or both (BiVAD). Some VADs are used temporarily in patients recovering from heart attacks or heart surgery, or waiting for heart transplant, while other are designed for long-term use in patients with advanced heart failure.
The MicroMed DeBakey VAD® unit pictured here, which is the result of a collaboration between NASA, Texas Medical Center Drs. Michael DeBakey and George Noon and MicroMed Technology, Inc., functions as a “bridge to heart transplant” by pumping blood throughout the body to keep critically ill patients alive until a donor heart is available. This VAD unit weighs just 4 ounces and measures 1 by 3 inches, making it ideal for children and small adults and less prone to infection than larger VAD units. Image courtesy of NASA.gov
Heart transplant is an operation in which the diseased heart is replaced with a healthy heart from a deceased donor. Heart transplant is a life-saving measure recommended for end-stage heart failure, when other medical treatments or less drastic surgery have failed.
Experimental Treatments and Research Trials
Ongoing research and clinical trials are leading to very promising new treatments for heart failure.
Researchers at Cedars Sinai Medical Center in Los Angeles have completed a groundbreaking clinical trial in which a patient’s own healthy heart stem cells were used to grow and repair heart tissue, reversing heart damage resulting from heart attack. This procedure involves creating healthy heart cells and then transplanting them into the heart, where they take up residence to improve the heart’s pumping ability. The hope is that this to research area will one day lead to growing entire hearts and other organs needed for transplant, eliminating the need for a donor organs and anti-rejection drugs.
Researchers at Sanford-Burnham Medical Research Institute in San Diego are developing a different approach to a similar end. This approach involves creation of a small molecule, or RNA [ribonucleic acid] therapeutic or other drug to simulate the heart’s ability to regenerate itself, thereby increasing the heart’s fundamental pumping ability.
Another recent breakthrough by researchers at Mount Sinai School of Medicine in New York, published in the Feb. 21, 2013 issue of the journal Circulation Research, used gene therapy to help repair heart damage resulting in heart failure. The Percutaneous Administration of Gene Therapy in Cardiac Disease (CUPID) trial used gene therapy to modestly improve symptoms in 17 patients with advanced heart failure. CUPID’s novel approach is designed to attract the body’s own stem cells to the damaged part of heart muscle to hopefully do repair work.
Participation in clinical trials involving new procedures or drug therapies may benefit heart failure patients, as well as people at risk of developing this debilitating disease. Depending on the goal of the clinical trial and status of the patient’s disease, heart failure patients may enter a clinical research study while continuing other treatments, but should discuss it with their cardiologist or other attending physician before signing up. A complete, worldwide list of current clinical trials for heart failure is available at the National Institutes of Health website. A list of Los Angeles-area research institutions conducting clinical trials for heart failure is available at clinicalconnection.com.
Monitoring and Self Care
Heart failure patients should be monitored closely by a cardiologist or attending physician, with check ups at least every three to six months. During follow-up appointments, tests to check the status of heart function are recommended.
Self-awareness of symptoms that indicate the heart failure is worsening can help improve patients’ quality of life and avoid hospitalization. Patients, therefore, should monitor their own heart rate, pulse, blood pressure, and weight at home and report any changes to their physicians. Weight gain over a day or two is especially important, as it is a sign of extra fluid retention and worsening of the heart failure. Limiting salt and fluid intake helps to prevent fluid retention
[See: Low Sodium Guidelines for Heart Failure].
Incidence and Survival Rates for Lung Cancer
According to the National Heart Institute (NIH), heart failure affects about 5.6 million Americans and is the primary cause of 55,000 deaths annually. But, it also contributes to cause of death in many more people. It was a contributing cause of death reported in 280,000 people [1 in 9 deaths] in 2008, according to NIH statistics. According to the NIH, about 50% of people with heart failure die within five years of diagnosis.
An estimated 400,000 to 700,000 new cases are diagnosed each year, according to statistics from the Ahmanson-UCLA Cardiomyopathy Center, which also notes that an estimated $8 to $15 million is spent each year on hospitalizations due to heart failure–more than double the amount spent on all forms of cancer combined. The UCLA center also reports that U.S. deaths associated with this disease has more than doubled since 1979, averaging 250,000 annually. The rise in heart failure cases is attributed to both an increase in the survival of victims of heart attack, which damages heart muscle, and rise in the incidence of obesity and diabetes nationally.
Related Information:
Simple Breath Test Might Diagnose Heart Failure
http://www.webmd.com/heart-disease/heart-failure/news/20130325/simple-breath-test-might-diagnose-heart-failure
Gene Therapy in Heart Failure
http://circres.ahajournals.org/content/102/12/1458
Video: Gene Therapy for Heart Disease
http://www.webmd.com/heart/video/gene-therapy-heart-disease
Heartening Results: The CUPID Gene Therapy Trial for Heart Failure
http://www.nature.com/mt/journal/v19/n7/full/mt2011123a.html
Walking to His Own Beat
http://www.discoveriesmagazine.org/walking-to-his-own-beat/
My Device: LVAD
http://www.discoveriesmagazine.org/my-device-2/
The Barath Cutting Balloon
http://www.discoveriesmagazine.org/from-inspiration-to-device/
10 Big Ideas
http://www.discoveriesmagazine.org/10-big-ideas/
The Genetics of Dilated Cardiomyopathy
http://discoverysedge.mayo.edu/dilated-cardiomyopathy/
Ties That Bind: Women’s Health, Heart Disease and Hormone Therapy
http://discoverysedge.mayo.edu/womens-health-research/index.cfm
Stem Cell Therapy for Heart Disease
http://my.clevelandclinic.org/heart/disorders/heartfailure/stemcells.aspx
Low-Sodium Guidelines for Heart Failurehttp://my.clevelandclinic.org/disorders/Heart_Failure/hic_Low-Sodium_Guidelines_for_Heart_Failure.aspx
Heart Failure Exercise Precautions – Exercise
http://my.clevelandclinic.org/disorders/Heart_Failure/hic_Heart_Failure_Exercise_Precautions.aspx
Potassium and Magnesium Supplements
http://my.clevelandclinic.org/disorders/Heart_Failure/hic_Potassium_Guidelines_for_Patients_with_Heart_Failure.aspx
Keeping Hearts Pumping
http://spinoff.nasa.gov/spinoff2002/hm_3.html
New heart failure trigger could change the way cardiovascular drugs are madehttp://beaker.sanfordburnham.org/2012/07/heart-failure-trigger-change-drugs/
References:
Children’s Hospital of Philadelpia
WebMD.com
National Heart Institute
Mayo Clinic
Medline Plus
American Heart Association
Healthinformation.com
NASA Spinoff
Wikipedia.com
Cedars Sinai Medical Center
Sanford-Burnham Medical Research Institute
American Nutrition Association
Ahmanson-UCLA Cardiomyopathy Center
American College of Cardiology
National Heart Lung and Blood Institute
U.S. Department of Agriculture