HomeDivisionsLung DiseaseLung Cancer
Lung cancer starts with the clustering of abnormal cells in the lungs, forming a malignant tumor. Unlike normal cells, malignant tumor cells grow without order and destroy surrounding healthy lung tissue.
A malignant tumor is dangerous because it grows uncontrollably and prevents other organs from working properly.
It may grow so large it blocks a major airway, making it difficult to breathe. Additionally, a cancerous tumor spreads to other parts of the body through blood and lymph.
Lymph is the fluid inside lymph nodes, the component of the immune system that filters foreign particles out of blood and then recirculates the white blood cells, the body’s defense against disease.
Lung cancer is the second leading cause of death in America after heart disease, killing 574,743 men and women in 2010, according to the Centers for Disease Control Prevention (CDC), and is the leading cause of cancer deaths.
It also is the most preventable form of cancer, as 80 to 90 percent of cases result from smoking tobacco.
Other risk factors for lung cancer include exposure to secondhand smoke, radon gas, asbestos, ionizing radiation, and other cancer-causing substances found in the home or workplace, as well as medical radiation to the chest and chronic lung diseases, like emphysema or chronic bronchitis. A family history of lung cancer also plays a key role in who gets lung cancer, as studies have linked mutations in several genes to this disease.
Types of Lung Cancer
The two common types of lung cancer are small cell and non-small cell, which are named for how the cancer cells look when viewed under a microscope.
Small Cell Lung Cancer
Small cell lung cancer only affects one in eight, or about 20 percent, of people with this disease. But it is the most aggressive and threatening type of lung cancer, because it metastasizes [spreads] quickly, usually within 90 days before symptoms appear or a diagnosis is made, to the liver, bones or brain.
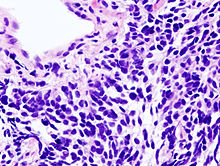
There are two forms of small-cell lung cancer: small cell carcinoma, or oat cell cancer, and mixed small cell/large cell cancer, or combined small cell lung cancer. These forms of small cell lung cancer also are named for the appearance of the cancer cells under a microscope. Both types originate in the large, central bronchi of the lungs, but grow and spread differently.
 |
|
Pictured is a microscopic view of a core needle biopsy of small cell lung carcinoma. Photo courtesy of Wikipedia.com. |
Non-small Cell Lung Cancer
Non-small cell is the most common form of lung cancer, accounting for about 80 percent of cases. Because this form of the disease spreads more slowly than small cell lung cancer, it may be effectively treated if caught early.
There are three types of non-small cell lung cancer, each of which begins in different kinds of cells and spreads in different ways. Each type is named for the kind of cells found in the cancer and how they look under a microscope.
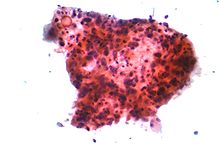
Squamous cell carcinoma, or epidermoid carcinoma, begins in squamous cells, which are the thin, flat fish-scale looking cells found in tissue that form the surface of skin and line hollow organs and the respiratory and digestive tracts.
 |
|
Pictured is a micrograph of squamous carcinoma. Photo courtesy of Wikipedia.com |
Large cell carcinoma begins in several types of large cells.
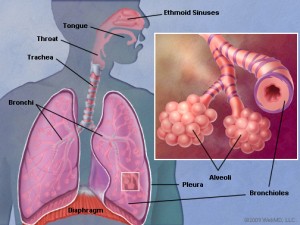
Adenocarcinoma is a form of lung cancer that begins in cells that line the alveoli Alveoli are tiny air sacs in the lungs at the end of the respiratory tree, where the exchange of oxygen and carbon dioxide takes place.
Less common forms of non-small cell lung cancer are: pleomorphic, carcinoid tumor, salivary gland carcinoma and unclassified carcinoma.
Signs or Symptoms of Lung Cancer
Symptoms of lung cancer are similar to other conditions, and sometimes victims of lung cancer do not experience any symptoms. However, a physician should be consulted if any of the following symptoms are present.
- Chest discomfort or pain
- A cough that doesn’t go away or gets worse over time
- Difficulty breathing
- Wheezing
- Blood in sputum (mucus coughed up from the lungs)
- Hoarseness
- Trouble swallowing
- Loss of appetite
- Weight loss for no known reason
- Feeling very tired
- Swelling in the face and/or veins in the neck.
Diagnosing Lung Cancer
The earlier lung cancer is diagnosed, the better the patient’s prognosis, or treatment outcome, which is why physicians routinely recommend an annual chest x-ray for smokers.
If symptoms of lung cancer are present, diagnosis begins with a physician exam and patient history that explores lifestyle habits like smoking, illnesses, medical tests, workplace or other environmental exposure to carcinogenic agents that present a risk for lung cancer.
The physician may then order one or more of the following diagnostic tests.
-
- Laboratory tests that test samples of tissue, blood, urine, or other bodily substances to help diagnose the disease, but also are used to plan and monitor treatment.
- Chest x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
<
- CT scan (CAT scan), or computed tomography, is an imaging procedure that makes a series of detailed pictures of areas inside the body from different angles, in the case of lung cancer, chest the chest area.
- Sputum cytologyis a procedure in which a pathologist views a sample of sputum, or mucus, from the patient’s lungs under a microscope to check for cancer cells.
- Fine-needle aspiration (FNA) biopsy of the lung involves removing a sample of tissue or fluid from the lung using a thin needle. CT scan, ultrasound, or another imaging procedure is used to locate the abnormal tissue or fluid in the lung. A pathologist examines the biopsied tissue or fluid under a microscope to look for cancer cells. The procedure may be followed with a chest x-ray to make sure no air is leaking from the lung into the chest cavity.
- Bronchoscopy involves insertion of a bronchoscope through the patient’s nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples to check for cancer cells. , which are checked under a microscope for signs of cancer.
- Thoracoscopy is a surgical procedure to examine organs inside the chest for abnormal tissue. The surgeon makes an incision between two ribs and inserts a thoracoscope into the chest. This thin, tube-like instrument has a lighted viewing lens and may also have a tool to remove tissue or lymph node samples, which are examined under a microscope for signs of cancer cells. In some cases, this procedure is used to remove part of the esophagus or lung. If targeted tissues, organs, or lymph nodes can’t be reached with the thoracoscope, thoracotomy, a larger incision between ribs to open the chest, may be required.
- Thoracentesis involves needle aspiration of fluid from the space between the lining of the chest and lung, which the pathologist examines to look for cancer cells.
- Light and electron microscopy involves examination of tissue samples under a high-powered microscope to look for certain changes to cells.
- Immunohistochemistry study is a laboratory test in which an antibody, dye, or radioisotope is added to a sample of cancer tissue to test for certain antigens. This test enables the pathologist to determine the type of cancer present.
Staging the Disease
Staging is the process used to determine if the cancer has spread, or metastasized, to other parts of the body. Cancer can spread to surrounding tissue or to other areas of the body through blood or the lymph system.
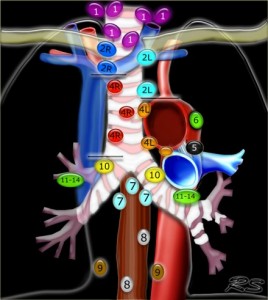 |
|
Pictured is the regional lymph node classification map for lung cancer staging, which was adapted from the American Thoracic Society mapping scheme. See map key for more information. Courtesy of the Radiological Society of the Netherlands |
The stage of the disease involves the size of the lung tumor, whether the cancer has invaded nearby tissue, such as the chest wall or has spread to lymph nodes or other parts of the body. The stage of the cancer, cancer type, symptoms and the patient’s general health will determine treatment options and the patient’s prognosis, or chance for recovery.
Prognosis and treatment decisions are based on the following information:
- The disease histology type;
- Tumor size and location;
- Involvement of pleura;
- Surgical margins, or normal tissue removed along with the tumor;
- Status and location of lymph nodes by station. [see lymph node map above];
- Tumor grade, a system used to classify cancer cells according to how abnormal they look under a microscope and how quickly the tumor is likely to grow and spread;
- Lymphovascular invasion or spread of cancer to blood vessels and/or the lymphatic system.
Tests to stage the disease
CT scan, or x-ray computed tomography, involves an x-ray machine linked to a computer that makes a series of detailed pictures of the chest, abdomen, brain and other parts of the body to determine if the disease has metastasized, or spread outside of the lungs. A contrast material, such as dye may be given by injection into the vein or by mouth, to provide more detailed images, making it easier to determine the tumor size and whether the cancer has spread to the liver, adrenal glands, brain or other organs.
PET scan, or positron emission tomography, is used to get an even better view of the tumor in the lung or to find cancer that has spread. With PET scan, a small amount of radioactive sugar is injected into the vein. The machine images sugar being used by cells. Cancer cells use sugar faster than normal cells, so the cancer cells look the brightest in the pictures.
MRI, or Magnetic Resonance Imaging, also can show whether the cancer has spread outside the lung. This machine uses a strong magnet linked to a computer to make detailed picture of the head and spine. Sometimes a contrast material, such as a dye, is injected to get a clear picture of the abnormal cells.
Bone scan is a nuclear scanning test that involves injection of a radioactive substance into blood vessels. The radioactive material travels through the bloodstream and collects in bones. A higher amount of the radioactive substance will collect in areas where cancer is present than in normal cells. This allows a scanner to detect, measure and image the cancer.
Other tests, such as biopsy of lymph nodes and other tissues or endoscopic ultrasound, may also be used to determine if the disease has metastasized to other areas of the body. EUS involves passing a miniaturized ultrasound probe though the mouth into the upper gastrointestinal tract to investigate organs and structures close to the lung, such as the esophagus, stomach, or duodenum.
Stages of Non-small Cell Lung Cancer
Occult Stage Lung Cancer – Tumor cells are found in sputum, but CT scan or other imaging tests do not find a tumor in the lung.
Stage o Lung Tumor – This stage is also called carcinoma in situ. This is a noninvasive cancer, in which abnormal cells are only found in the innermost lining of the lung.
Stage I Lung Cancer – The lung tumor is not more than 5 centimeters (two inches), or about the size of a lime, and has grown through the innermost lining of the lung into deeper lung tissue, but has not invaded nearby tissues, such as the chest wall, or spread to lymph nodes.
Stage II Lung Caner – – The tumor is smaller than 7 centimeters across, and cancer cells have spread to nearby lymph nodes. Or the tumor is more than 5 centimeters across or has invaded nearby tissues, such as the chest wall, diaphragm, pleura, main bronchus or tissue around the heart, but has not spread to lymph nodes.
Stage III Lung Cancer – The tumor may be any size, but more than one malignant tumor is found in the lung. Cancer cells may also be found in lymph nodes on either side of the chest or neck or may have invaded nearby organs, such as the heart, esophagus or trachea.
Stage IV Lung Cancer – The cancer has crossed mediastinum, the space between the lungs, invading lymph nodes in nearby tissues, as well as the mediastinum. Malignant tumors are now found in both lungs, or the cancer has spread to other parts of the body, such as brain, bones, liver or adrenal glands, or cancer cells are found in fluid between the layers of pleura.
Stages of Small Cell Lung Cancer
Physicians commonly use a two-stage system to describe the status of small cell lung cancer: limited stage and extensive stage. Staging small cell lung cancer in this way helps to separate patients who may benefit from the more aggressive treatments [limited stage], like a combination of chemotherapy and radiation, from those for whom treatments are unlikely to cure the disease [extensive stage].
Limited- Stage Lung Cancer means the cancer is only in one side of the chest. This can include one lung and the lymph nodes on the same side of the chest, including lymph nodes above the collarbone, or clavicle, as long as they are on the same side of the chest as the cancer. Lymph nodes at the center of the chest, or mediastinal lymph nodes, also may be included in a limited-stage diagnosis, even when they are closer to the other side of the chest. The chief consideration of a limited-stag diagnosis is the cancer is confined to a small enough area with one radiation therapy port.
Extensive-Stage Lung Cancer means the cancer has spread to the other lung and lymph nodes on the other side of the chest, or to distant organs, including the bone marrow. This stage also refers to the spread of fluid with small cell lung cancer cells to surrounding tissues. Because this type of lung cancer spreads quickly, often before symptoms appear or a diagnosis is made, about two out three victims of small cell lung cancer have extensive disease.
Treatment of Lung Cancer
Surgery, or lobectomy, is an option for people with early-stage lung cancer. Surgery for lung cancer involves removal of the part of lung, or lobe, that contains cancer. Depending on the extent of the cancer, the surgeon may remove the tumor and some of the surrounding tissue, but not the whole lobe, or the entire lung. Nearby lymph nodes are also removed.
Following surgery, air and fluid collect in the lungs, so a chest tube is inserted during surgery to allow the fluid to drain. The chest tube is removed several days after surgery. Coughing and breathing exercises performed several times a day help to remove fluid from the lungs.
Radiation Therapy is an option for any stage of lung cancer. People with early-stage lung cancer may opt for radiation therapy in place of surgery. It may also be used following surgery to destroy any cancer cells that are still present in the chest or to shrink a tumor blocking the airway. For advanced lung cancer, radiation is used in combination with chemotherapy. Radiation therapy also can be used relieve pain caused by lung cancer. It also is used to treat lung cancer that has spread to the brain.
With radiation therapy, high-energy rays are aimed at the tumor to kill the cancer cells. The radiation only affects cells in the area treated. Treatments most often are done on an outpatient basis five days a week for about six weeks.
Treatments are painless, but patients may experience side effects, depending on the intensity of the radiation. Possible side effects include sore throat, cough, shortness of breath, difficulty swallowing, or a burning sensation in throat or chest. Skin in the chest area may become red and dry or get darker, and may feel tender or itchy. When treatment is completed, side effects usually disappear. Patients may also become tired during radiation therapy, particularly in the later weeks of treatment.
Chemotherapy may be used alone or in combination with radiation therapy or following surgery to kill cancer cells. Treatment involves giving drugs intravenously–injected into a vein–and is generally administered in a clinic or doctor’s office.
may be used alone or in combination with radiation therapy or following surgery to kill cancer cells. Treatment involves giving drugs intravenously–injected into a vein–and is generally administered in a clinic or doctor’s office.
Chemotherapy drugs kill cancer cells, but also harm normal cells that divide rapidly, including blood cells, cells in hair roots and cells that line the digestive tract. These drugs often lower the level of healthy blood cells, making the patient more susceptible to infections, bruise or bleed easily, and feel weak and tired. If the patient’s blood cell count gets too low, the chemotherapy dose may be reduced or treatment stopped temporarily. Medications may also be given to help step up production of new blood cells.
Other side effects include hair loss, poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Medicines, including both pharmaceuticals and/or herbal supplements may help to relieve unpleasant side effects. For example, ginger, fennel or mint may be recommended to help relieve nausea associated with chemotherapy and radiation.
The intensity of side effects depends on the chemotherapy drugs used and dosage given. When treatment is discontinued, however, side effects disappear and hair grows back.
Targeted Therapy uses chemotherapy agents specifically designed to selectively target molecular pathways that are responsible for or substantially drive the malignant phenotype of lung cancer cells. Targeted agents are selective in their effects by modulating the activity of proteins necessary and essential for oncogenesis–the process by which normal cells become cancer cells–and maintenance of cancer, especially enzymes driving uncontrolled growth and spread of malignant tumors. As a result, there are fewer toxic effects on normal cells, and patients experience less troubling side effects, particularly less nausea, vomiting, death of cells in bone marrow and the gastrointestinal tract, while getting increased effectiveness against tumor cells.
Clinical Trials
Continuing cancer research is advancing more effective treatments for lung cancer, as well as may help in early diagnosis and prevention. Clinical trials often are the last hope for patients with advanced lung disease. However, patients with any stage of lung cancer patients may want to explore new treatment options under investigation and/or participate in clinic trials.
Lung cancer patients can enter clinical before, during or after starting cancer treatment, depending on the goals of the clinical trail and patient status. The NCI provides a current, worldwide list of clinical trials at http://www.cancer.gov/clinicaltrials. Los Angeles-area research institutions conducting cancer research include: UCLA Jonsson Comprehensive Cancer Center, USC Norris Comprehensive Cancer Center, Cedars Sinai Samuel Oschin Comprehensive Cancer Institute, Saint John’s John Wayne Cancer Institute, and City of Hope Beckman Research Institute.
Nutrition
Good nutrition is essential before, during and after cancer treatment. Patients should eat the right amount of calories to maintain a healthy weight, including enough protein to maintain strength. Lung cancer patients should consult with a registered dietitian or nutritionist who specializes in nutritional planning for cancer patients.
Follow-up Care
Lung cancer patients require regular checkups following treatment to identify any suspect changes in health that indicate a recurrence of the cancer. But, patients who experience any health problems or cancer symptoms between checkups should contact their physician immediately.
Lung cancer may return in the chest or another area of the body. Regular checkups help to ensure the physician detects and treats a recurring cancer early before it spreads. Checkups include physical examination, blood test and/or CT scan.
Incidence and Survival Rates for Lung Cancer
The chance for both men and women developing lung cancer during their lifetime is 1 in 14. More than 160,000 Americans died of lung cancer in 2012, and an estimated 228,000 new cases will be diagnosed in 2012, according NCI SEER (Surveillance Epidemiology and End Results) statistics. Additionally, nearly 373,500 Americans are living with lung cancer today.
Survival rates are relative to type and stage of lung cancer, but may differ according to race and sex. The overall five-year relative survival for 2002-2008 from 18 SEER geographic areas was 15.9%. Five-year survival by race and sex was: 14.1% for white men; 18.7% for white women; 11.8% for African-American men; and 14.6% for African-American women.
|
Stage Distribution and 5-year Relative Survival by Stage at Diagnosis for2002-2008, |
||
|
Stage at Diagnosis |
Stage Distribution (%) |
5-year Relative Survival (%) |
| Localized (confined to primary site) |
15 |
52.2 |
| Regional (spread to regional lymphnodes) |
22 |
25.1 |
| Distant (cancer has metastasized) |
56 |
3.7 |
| Unknown (unstaged) |
6 |
7.9 |
The stage distribution is based on NCI Summary Stage 2000. (See NCI Fast Stats for more detailed statistics.)
RELATED INFORMATION:
Tofu-Rich Diet May Help Women With Lung Cancer
http://www.webmd.com/lung-cancer/news/20130326/tofu-rich-diet-may-help-women-with-lung-cancer-live-longer
Gene Test May Help Determine Early Lung Cancer Survival
http://www.webmd.com/lung-cancer/news/20120126/gene-test-may-help-determine-early-lung-cancer-survival
Microwave Technique Fights Lung Tumors
http://www.webmd.com/lung-cancer/news/20111128/microwave-technique-may-fight-lung-tumors
Drugs That Control Genes May Treat Lung Cancer
http://www.webmd.com/lung-cancer/news/20111109/drugs-that-control-genes-may-treat-lung-cancer
WebMD.com Cancer Channel
http://www.webmd.com/breast-cancer/video/silver-cancer-treatment-pain
UCLA Cancer Researchers Develop ‘Liquid Biopsy’
http://www.empowher.com/cancer/content/ucla-cancer-researchers-develop-liquid-biopsy
6 Ways to Keep Cancer at Bay
http://www.huffingtonpost.com/maria-rodale/6-ways-to-keep-cancer-at_b_2781063.html
Expanding the Playing Field: Immune-Based Therapy Shows Potential for Lung, Other Cancers
http://www.cancer.gov/clinicaltrials/results/summary/2012/PD-1-immunotherapy0612
Chemotherapy Combination Improves Survival in Elderly Lung Cancer Patients
http://www.cancer.gov/clinicaltrials/results/combochemo-NSCLC0610
Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials
http://www.ncbi.nlm.nih.gov/pubmed/21144578
Cetuximab Plus Chemotherapy Extends Survival for Advanced Lung Cancer
http://www.cancer.gov/clinicaltrials/results/summary/2010/cetuximab-NSCLC1210
Palliative Care Improves Survival, Quality of Life in Advanced Lung Cancer
http://www.cancer.gov/clinicaltrials/results/summary/2010/early-palliative-care0910
Learn About Clinical Studies
http://clinicaltrials.gov/ct2/info/understand
Nutritionist: ‘Eat to Win’
http://www.jewishjournal.com/health/article/nutritionist_eat_to_win
Find Clincal Trials
http://clinicaltrials.gov/ct2/home
Eating Hints: Before, During and After Cancer Treatment
https://www.cancer.gov/publications/patient-education/eating-hints
Top Cancer-Fighting Foods
http://www.webmd.com/cancer/ss/slideshow-cancer-fighting-foods
What You Need to Know About Lung Cancer
https://pubs.cancer.gov/ncipl/detail.aspx?prodid=P026
Soybean Meal Peptides Could Stop Colon, Liver And Lung Cancer Growth
http://www.huffingtonpost.com/2013/03/24/soybean-cancer-colon-liver-lung-meal-peptides_n_2916645.html
FoxM1 Is Associated with Poor Prognosis of Non-Small Cell Lung Cancer Patients through Promoting Tumor Metastasis
http://www.ncbi.nlm.nih.gov/pubmed/23536876
Facing Forward: Life After Cancer
http://www.cancer.gov/cancertopics/coping/life-after-treatment
Follow-up Care After Cancer Treatment
http://www.cancer.gov/cancertopics/factsheet/Therapy/followup
References:
National Cancer Institute
National Institutes of Health
American Cancer Society
Wikipedia.com
UCLA
American Lung Association
WedMD.com
MedlinePlus.com
Cancer Treatment Centers of America